The challenges of universal health coverage in sub-Saharan Africa: permanence and failures of New Public Management instruments
Valéry Ridde
Achieving universal health coverage (UHC) by 2030 is now a health goal recognised and pursued by the international community and member countries of the World Health Organisation (WHO)[1]. According to the WHO, its objective is « to ensure that all people have access to the health services they need without financial hardship to users »[2]. Since its inclusion in 2015 as a target in one of the United Nations’ Sustainable Development Goals (SDGs), achieving this goal has become the talk of many. However, realizing this goal is complex as UHC is a multidimensional concept that can be viewed from legal, humanitarian, public health, economic or social perspective (Abiiro & De Allegri, 2015). Advocacy groups have been formed to uphold this objective (www.uhc2030.org). International programmes have been set up to support countries in policy dialogue to achieve this (https://www.uhcpartnership.net) (Robert et al., 2019). Bilateral projects (Belgian, Japanese, French, etc.) have been established to further test and implement interventions specifically dedicated to its pursuit[3]. Experts and technical assistants have been deployed to advise policymakers[4]. And finally, research teams are still trying to understand how to strengthen UHC based on evidence (https://www.unissahel.org) and which instruments are most relevant[5] to move towards UHC. Despite all these efforts, as I will try to demonstrate in the rest of this introduction, most of the instruments tested in the last 10 years are part of the tradition and ideology of New Public Management (NPM). The long, quiet river of this approach continues to flow, without resistance despite its ineffectiveness. However, it seems to me that the understanding of the challenges of UHC and the possible choices to achieve it is not yet sufficiently shared and understood, especially in the French-speaking world in which the authors gathered in this collective navigate in.
The need to make scientific knowledge on UHC accessible
This book, therefore, aims to make the most out of recent research on UHC in sub-Saharan Africa by increasing its accessibility to a larger number of people by publishing it in French, free of charge. Its objective is greater sharing of knowledge and dissemination of lessons learned from the reforms undertaken. Many of the chapters are adapted translations of articles published in English-language scientific journals, which few officials take the time to search for and read[6], and which pose as a language-barrier. Scientists looking for methods can refer to the corresponding articles from which these chapters were taken. However, it should be emphasized and this is a strength of the book, that the vast majority of the chapters are based on the use (a priori or a posteriori) of conceptual frameworks or theories derived for the most part from the social sciences and research on health policies and systems (Gilson, 2012; Robert & Ridde, 2016). We know, however, that this type of usage is not yet commonplace in African research (Jones et al., 2021). This book, therefore, contributes to a more systematic use of these theories and conceptual frameworks to strengthen the quality of studies from a comparative perspective (Ridde, Pérez et al., 2020). Our collective effort is aimed at democratising knowledge or, to put it in a more scholarly way, in achieving epistemic justice. Thus, we must salute the commitment of Florence Piron’s team and the publishing house Science et Bien Commun, as well as all the authors whom have agreed to dedicate their time to these translations and to the corrections that I have too often requested. I, therefore, hope that French-speaking people around the world will be happy to read these scientific analyses of the issue of UHC in sub-Saharan Africa. This book is even more essential as a recent analysis of the main publications on UHC in the world shows a total absence of French-speaking teams. From 1990 to 2019, none of the 19 most prolific research institutions on UHC was francophone and none of the countries in sub-Saharan Africa, excluding South Africa, were among the most studied on the subject (Ghanbari et al., 2021). This confirms the compelling need to conduct and share research in French.
Instead of presenting each of the 28 chapters individually, of which summaries are available at the end of the book, to understand their contents, I thought it more relevant to offer, based on the texts gathered in this book, a global reflection on the past and contemporary history of UHC in this region of the world. The book’s originality lies in the presentation of recent health systems reforms organised in certain sub-Saharan African countries in four main sections, classically developed in the study of public policies: emergence, implementation, effects and perspectives. To our knowledge, this grouping of articles essentially centre on the function of health financing, even though the other dimensions of health system performance underlie most of these initiatives, adds a new stone to the construction of the history of reforms. In this introduction, after presenting the context of the UHC, I will attempt to synthesise the knowledge that we are collectively updating in this book. This will be done by generalising through a cross-sectional analysis of the chapters on some elements that I consider key to understanding the contemporary situation of UHC and NPM instruments (notably direct payment and results-based financing).
The challenges of UHC in sub-Saharan Africa
It must be acknowledged that UHC as « the most powerful concept that public health has to offer », as said by the former WHO Director-General, has difficulty in becoming a reality for a majority of the sub-Saharan population. It is certainly far from being a « global public good », whose ambiguities and close links between health reforms in West Africa and the NPM were already shown by Bruno Boidin (2014). Every day, the media and people in sub-Saharan Africa undergo painful experiences that are quickly forgotten in high international and national circles. Examples of such experiences include a woman who could not give birth in a hospital because of the lack of an ambulance, a child who could not get a rapid diagnostic test for malaria, and further afield, a man who could not pay for a check-up to ensure that he did not have prostate cancer. Every day, sub-Saharan families struggle to find the financial, human and relational means to treat themselves. All these families, regardless of their socio-economic level, face this same challenge. But of course, it is always the poor and most isolated people who are the most forgotten and least able to overcome these barriers[7], further ensuring the persistence of social inequalities in health. These inequalities however, are not unique to sub-Saharan Africa, but widely experienced throughout the world. For example, the denial of care and racism experienced by migrants in Canada (Ridde, Aho et al., 2020) is no different from the dramatic situation of the indigent in Burkina Faso[8] whose mental health is failing (Pigeon-Gagné, 2021); or the ethno-cultural mobilisations to justify the challenges of access to care for women in certain regions of the country (Belaid et al., 2017).
This transversality of realities experienced by people seeking care in the North and the South gives complete meaning to the concept of global health (Ridde & FIllol, 2021). Following Adesky (2017), I believe that the concept of the « subaltern »[9], first enunciated by Antonio Gramsci and then widely developed by Southern thinkers, is relevant in understanding situations experienced by some people in the North. It also applies to the indigent (in the North and South), who have continually been excluded from health systems (V. Ridde & Jacob, 2013). However, to my knowledge, the concept of ‘subalternity’ has not yet been invoked to understand the challenges of those who have to forego care due to lack of financial means, among other things. In considering the possibility of analysing the issue of access to health care for the poor in sub-Saharan Africa, the mobilisation of subalternity could certainly make it possible to bring to light not only the well-known situations of precariousness, but also the challenges of stating and claiming the right to health care access for these people. Albeith not necessarily invisible, they indefinitely remain the great forgotten of health reforms despite the recurrent international and national speeches promising the inclusion of all and claims of not wanting to leave anyone behind (Louart et al., 2020; Ridde et al., 2019). The history of public policies and official development assistance show that « policies intended to be pro-poor are likely to be watered down so as to include some benefits for the better-off, and/or to have those benefits diverted away from the poor during implementation » (Brinkerhoff & Brinkerhoff, 2013 : 381).
A return to less technical analyses of the UHC (particularly on modes of financing or contracting, as we shall see below) which is more focused on the values of solidarity and the global public good should be mobilised (Mladovsky et al., 2015; Prince, 2017). Is it not the time to analyse health systems from a postcolonial perspective? to describe them « no longer on the basis of the principles (of justice, of social integration) that are supposed to regulate domination, but on the basis of the very experience of domination, particularly on the basis of the dominations weighing on the subaltern social situations » (Renault, 2008). This situation is experienced by the poorest people excluded from health care systems in sub-Saharan Africa (and elsewhere in the world)?
However, these individual stories which could be heard every day if we were to truly listen, are not merely words, but are rather the daily reality for many and, above all, are narratives reflected in the statistics and figures that international organisations constantly feature. Table 1 presents some indicators for the countries covered in this collective work, as well as a comparison, by way of illustration, with Canada and France[10].

In reading the chapters of this collective work, it appears to be that medicine has not improved in terms of hospitality since the unambiguous observations made 20 years ago (Jaffré & Olivier de Sardan, 2003). Beyond the stigmatisation of professions that the title of this long-standing study carried out in French-speaking West Africa by a team of anthropologists would lead us to believe, a deeper, more structural and complex problem remains and seems to make the idea of UHC utopian, as well as perpetuating the challenges of improving access to care. Following Didier Fassin (2000) who more than 20 years ago denounced the rhetoric that effective public health is achieved more with words than with actions, we can still ask ourselves today why all the verbal commitments and written international declarations fundamentally fail to materialise, and ultimately improve the lives of the majority of people living in sub-Saharan Africa whose health needs remain mostly unmet. Nevertheless, many lessons can be drawn from the initiatives that have been launched, such as the mutual insurance schemes that have become compulsory in Rwanda[11], the professionalisation of departmental mutual insurance schemes in Senegal[12] and the exemption from payment for care in Burkina Faso[13]. However, the « small steps » that policy-makers tend to analyse seem to go slowly (not to say backwards). The lessons learned seem to travel poorly (Olivier de Sardan, 2021), unlike ready-made intervention models (Olivier de Sardan et al., 2017). Effective and equitable public policy transfers (Rose, 2005) are rare and difficult given that everyone is pushing for the solution they believe in so strongly, as the cover of this book seeks to show.
Recurrent failures of the NPM and reliance on the instrument pathway for the UHC
I must start this section with an old personal memory. In 1999, after several years of coordinating projects for NGOs in Asia and West Africa, I decided to go back to school and start a master’s degree in community health (not so much public health) at Laval University in Quebec (Canada). During my first « international health » course, since the concept of global health was not yet in use (Ridde & FIllol, 2021) even though the microbial unification of the world was taught to us by an important Quebec book (Gélinas, 2000). Professor (Jacques Girard) imposed on us the reading of the famous 1993 World Bank report on world development: « Investing in Health » ((World Bank, 1993). I wondered why I had to spend time reading this long document which content was framed by a worldview far removed from the realities I had observed in the field. This report is notably famous for its advocacy of efficiency (in line with the WHO (WHO Study group, 1978)) as a criterion for choosing interventions, and thus reinforces the place of the economic criterion in the selection of effective actions. This is a concept which seems to persist (Hayati et al., 2018). This is less well known or explained, but, it has also been the continuation of a monumental fiasco in the promotion of policy instruments (Howlett, 2011) of New Public Management. To be honest, I had completely forgotten this report (following the 1985 report (De Ferranti, 1985)), suggested that countries should engage in health financing policies through direct payment for care by service users (user fees). Curiously, this same report is still being invoked in 2020 by NPM ideologues, who are now defending[14] strategic purchasing (infra) as an instrument (without citing any supporting evidence) for achieving health as a global common good (Soucat & Kickbusch, 2020). This reappraisal of the theses supported by the World Bank 25 years earlier confirms the permanence of the solutions (path dependency, as per political scientists) carried by a few political entrepreneurs navigating between international organisations.
At this point in the introduction, it is useful to return to the definition of NPM in the context of health reforms in Africa in particular. Recall that Kaul (1997 : 14) defined NPM, in the context of liberalising economies, as « As government moves from a concern to do towards a concern to ensure that things are done ». This was the World Bank’s vision of the role of the state in health at the time of the launch of its 1997 health, nutrition and population strategy (Abbasi, 1999). Bruno Boidin (2014 : 153) reminds us that « The anti-statism that dominated the 1980s and 1990s largely favoured the partial privatisation of health systems and health aid ». The neo-liberal view of the economy (which the PBF claims and « there is little doubt » says a former World Bank consultant (Falisse, 2019 : 99)) suggests that the lack of competition and competition are the main problems of the public sector. Indeed,
To the historian, global health appears as both response and adaptation to a new situation dominated by a neoliberal agenda, associated with the rise of the World Bank alongside (and sometimes displacing) the WHO in the area of health, the quantification of health as an economic factor, the generalization of public-private partnerships and alliances independent from the UN system and the call for mobilizing « civil society » rather than nation-states. (Gaudillière et al., 2020 : 3)
One of the first collective analyses of these reforms for the health sector in the South was published in 2001 (Mills et al., 2001). It recalled that the NPM is manifested in three fundamental dimensions: responsibility, accountability and performance. Table 2 shows the relationship between the NPM and health sector reforms of the 1990s under these three dimensions.

The analysis in Table 2 clearly shows how these instruments, directly associated with the NPM, persist in the policies and interventions of the 2010s studied in this collective book (in bold in the table). If community-based mutuals were not mentioned, it is because they were not present in the countries concerned by this study (Ghana, Zimbabwe, India, Sri Lanka, Thailand), since this instrument remains a very West African specificity with a few attempts in Central Africa (Waelkens et al., 2017). However, these community mutuals (CBHI)[15] apply certain NPM instruments, such as direct payment (by users at the point of service delivery) and contracting[16][17], which remind us of the paradoxical need for a strong state for governance of these processes (Boidin, 2014). Furthermore, to ensure a better comparison between countries in their analyses, the researchers chose to focus on four emblematic reforms of this NPM approach, including direct payment and contracting (Mills et al., 2001). These are at the heart of the chapters in this book.
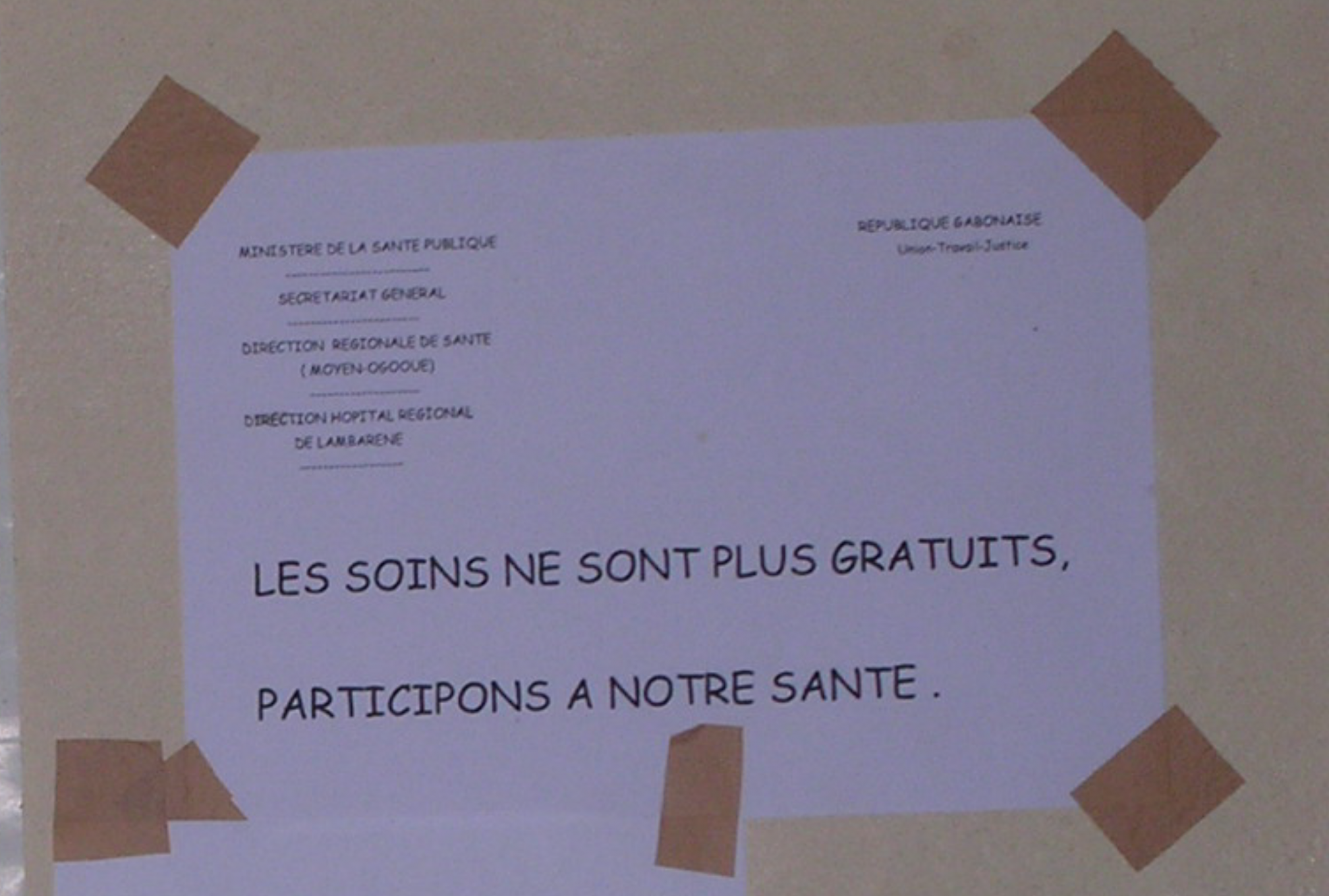
Today, it is likely that the majority of people in sub-Saharan Africa who are unable to afford treatment, or who are detained against their will in hospitals because they cannot pay their bills (Handayani et al., 2020) that their situation is partly due to the views of some of their national officials and experts from international organisations who remain convinced of the importance of « participating »[18] by paying at the point of service (photo Gabon). In many African countries, less than one in two children with pneumonia still seek professional care (Table 1). By referring to this 1993 report promoting the Bamako Initiative (an emblematic reform of the NPM, notably through the generalisation of user fees (Gilson et al., 2000)), the fervent defenders of strategic purchasing (Soucat & Kickbusch, 2020) does not seem to have been effective in Europe (Klasa et al., 2018), turn a blind eye to a significant body of research that has shown the Initiative’s lack of relevance and the exclusion from access to care that it has engendered by recommending it (Ridde, 2011). Community management of the funds contributed by the few users has also not been very successful (Balique et al., 2001; McCoy et al., 2012). Faced with this heresy, Amnesty International, which was not known for its specific involvement in the field of health, even decided in 2009 to write its first report in this area (Amnesty International, 2009) by attempting to influence the decisions of a West African state[19]. At the time, a professor of gynaecology countered Amnesty International’s proposals by publicly asserting before his peers that if childbirth were made free, women would have more children, thus helping to propagate the conventional wisdom (Ridde & Ouattara, 2015) the « overuse » of free health services. This doctor was later appointed Minister of Health. History will tell whether he will decide to make his decisions on a scientific basis, rather than an ideological basis[20]. This appointment shows once again that ideas endure, even if they run counter to research evidence. It was not until the COVID-19 pandemic that in foxes influenced policymakers (Ridde et al., 2014). Canadian economists proposed the same year as the World Bank report to compare user fees to zombies (Evans et al., 1993) which shows that evidence of the unfairness and inefficiency of direct payment has been available for a long time, beyond Africa (Batifoulier, 2013). The history of direct payments[21], written elsewhere (Ridde, 2015) will not be revisited. It took more than 20 years for some economists in these influential international institutions to publicly admit their mistakes (Paganini, 2004; Rodin & De Ferranti, 2012). Yet, all the evidence was available against this proposal, whose foundations are to be found in the NPM theses. Similarly, after decades of projects for the organisation of mutual health insurance with voluntary membership, a co-payment and community management[22], the actors of this movement have disappeared from the international scene, although many countries, such as Senegal or Mali for example (Deville et al., 2018), continue to believe in it but are beginning to test other approaches (for example, professionalisation in Senegal (Bossyns et al., 2018)). The issue of solidarity, which was highlighted as one of the characteristics of community mutuals (CBIH), has largely stumbled on the erosion of this value in a globalised Africa (Mladovsky et al., 2015; Roth, 2012; Soors et al., 2013; Vuarin, 2000) and of disease risk sharing that cannot be financially viable at this miniscule scale (Bossyns et al., 2018) in an overly fragmented health financing system (Mladovsky, 2020). This is one of the reasons for current attempts to scale up, as being tested by Mali and Senegal.
From street-level workers to second-line actors
Today, the tide seems to have —somewhat— turned and no one would dare —publicly for a long time— (Robert & Ridde, 2013) in development banks, international organisations and —somewhat less so— among African leaders mention the use of direct payment as a solution for financing health systems. But keeping quiet about it, no longer writing it into project documents, and acquiescing to the policy statements of international[23] organisation leaders does not mean that the ideas; and reasoning do not continue to be firmly embedded in the minds of policymakers. While these people are undoubtedly the frontline actors who shape and implement policies (Lipsky, 2010) concerning this issue of direct payment (Béland & Ridde, 2016), it also the case for the experts —African or not— involved upstream in the formulation and framing of health interventions (i.e. second-line people). These people, whom Lara Gautier (2018) has described as dissemination entrepreneurs, are very often at the heart of decisions about the content of health policies in African countries dependent on international aid. What Lara Gautier’s (2018) thesis also shows very well is that this influence is by no means confined to Western spheres and experts. Their colleagues in African countries —economists or public health doctors trained in certain health economics— also participate in the dissemination and permanence of ideas and policy instruments[24]. This situation contributes —in part— to explain the low level of ownership of UHC solutions by African governments (Gautier & Ridde, 2017). If this book only mentions at the margin —by focusing on their impacts because it was necessary to leave time for this evaluation— the policies of exemption from payment for care, whose implementation challenges were presented in a previous book on the Sahel (Olivier de Sardan & Ridde, 2014) is precisely because this instrument of the NPM and the financialisation of health[25] (user fees) has been eclipsed in favour of another during the last decade: results/performance-based financing (PBF). The latter therefore has a prominent —and de facto— empirical place in our collective.
Indeed, after direct payment and its recurrent failures, another instrument that has been shamelessly tested over the last ten years in the region is the PBF (for its testing in Asia, see for example the case of Afghanistan that I had analysed (Ridde, 2005)). It can be understood as a continuation of the contracting and outsourcing of services approaches of the 1990s, the failures of which were highlighted (Mills et al., 2001). While direct payments —the instrument of the NPM— went out the window (rhetorically, as they are still largely present), it is through the door —programmatically and with huge international funding— that the PBF has been sought (Paul, Albert, et al., 2018). However, its many implementation challenges,—which the book’s chapters describe— its dependence on international donors, the perverse effects it generates (Turcotte-Tremblay et al., 2018); and its dubious effectiveness (Gage & Bauhoff, 2021) certainly explained by its lack of theoretical justification ((Paul et al., 2021) make the PBF less and less proposed and imposed. Recently, it is another term that the WHO and others are seeking to introduce through another door in health systems: strategic purchasing. This may be the subject of our next book.
With the arrival of the PBF in recent years, two remarkable dimensions should be highlighted. On one hand, despite the knowledge of the injustice of direct payment driven by the NPM, it has hardly ever been questioned by international organisations and specialists —Western and African— who have influenced states to organise the PBF. On the other hand, the current discursive transformation of the BRF into strategic procurement —which would be a broader concept than the BRF— is a logical ideological pursuit. In recent years, therefore, we have been faced with a twofold permanence of the choice of instruments anchored in the NPM. Here we are at the heart of what « Linder and Peters called them « instrumentalists » said they would select the same instruments regardless of the circumstances. Many of these decision makers had strong disciplinary backgrounds » (Veselý, 2021 : 10). In the case of the PBF, Lara Gautier has shown that the disciplinary influence of orthodox[26] economics was a major factor in the diffusion of ideas (Gautier, Coulibaly, et al., 2019). In Mali, for example, Dutch and Malian consultants promoting the PBF in the 2010s —before the arrival of the World Bank— made it clear in their training manuals that « health care delivery is seen as a market product rather than a public good » (Fillol et al., 2020 : 119). Vesely (2021 : 2) rightly proposes, with the concept of autonomy of individuals’ attitudes towards policy instruments, that:
individuals (be they decision makers, public officials or citizens) have attitudes not only toward policy problems and policy goals but also toward the means by which these problems are to be solved and goals attained, and that these attitudes toward policy instruments are relatively stable over time and independent of particular policy issues.
The situation we describe in this book, therefore, shows the agility of these people and organisations that are not very open to criticism and evidence that goes against their ideas (cognitive dissonance). To illustrate my point in another way, it should be noted, for example, that in the WHO’s 15-page Policy Brief on strategic purchasing; 37 references are cited in support of the promotion of the instrument, 14 of which were written by people from the WHO and nine from the World Bank. This leaves little room for divergent ideas. Moreover, no critical references are cited in this note (Inke Mathauer et al., 2019). Regarding the lack of consideration for research findings challenging dominant ideologies, we have shown elsewhere how the World Bank has politicised the evidence on PBF (Gautier & Ridde, 2018). We recall the use of PBF in Rwanda[27] as a strategy of « cherry-picking (learning only from the « best model ») that leads to overconfidence in a standard model » (Gautier & Ridde, 2018) as well as the instrumentalisation of impact assessments, and the presence of major conflicts of interest. WHO health economists have an editorial in the WHO newsletter (McIsaac et al., 2018). The WHO newsletter refused to publish our response demonstrating this misinterpretation. The highly subjective selection of sources and data disseminated had already been noted in another WHO note on exemptions from payment for care (Mathauer et al., 2017). It ignored a significant part of the evidence that showed the relevance —and challenges— of this instrument, which is not surprising since the authors are known to be in favour of the PBF. Like the World Bank, the WHO and its experts are therefore not exempt from the influences and directions of the debate on health financing instruments[28] and equity issues in particular. A recent analysis points to the fact that the WHO’s discussions on the issue of equity « are highly ambiguous, inadequate, and contradictory, which has led some scholars to question the normative position held by the WHO » (Amri et al., 2021).
The role of ideas is permanent (Béland & Cox, 2011) and so is the challenge of collaboration between the world of research and that of decision-making[29]. For example, in 2019, the WHO Regional Office for Africa and the P4H network organised a workshop on UHC with decision-makers from the Sahel in a city in Senegal without inviting a research team. At the same time, several teams were in a hotel room a hundred metres away, also for a workshop on UHC. A few months later, the (Western) head of the organisation explained to me that not inviting research teams had been a deliberate choice.
Returning now to the issue of PBF, the analysis shows surprisingly that almost all of the tens of millions of dollars —often distributed in the form of loans that African taxpayers will have to pay back one day— invested with Western and/or African technical support in these projects in Africa have been focused only on strengthening the supply of care (mostly through staff bonuses and new and unsustainable funding to health centres); forgetting the —yet widely known— challenges of the population to pay the fees claimed. Very few PBF projects have attempted to remove (or combine PBF and exemption) these direct payments for all, whereas the Cambodian experience for example (Van de Poel et al., 2016 : 99), which is well known to advocates of this approach, has shown the relevance of this dual approach. If « the hybrid nature of the PBF associated with the exemption in Burundi is absent from current academic research », it is not because it « focuses on measuring the effects and perverse effects of the PBF on the use of care and its quality » (Falisse, 2019 : 99) which seems a necessary evil given the resources devoted to this instrument; but it is because no other country has really engaged in these « hybrid » solutions for essentially ideological reasons and influences.
The perception of the problem (to speak as Bacchi whose approach is used in the chapter by Gautier et al.) of access to care guides the solutions. In the case of the PBF, economists or public health experts trained in orthodox health economics (Gautier et al., 2018), believe that the main problem faced by people in Africa with ill health is the lack of motivation of staff, which could be improved using a financial bonus and ultimately lead to a better quality of health care. The complexity and the holistic and systemic vision of health systems are thus often sidelined in favour of a simplistic vision, and a theoretical approach with little empirical basis (Paul et al., 2021). Very few PBF projects such as in Burkina Faso or Benin have agreed to abolish out-of-pocket payments for some care. But, this was only possible for the poorest (here we return to the ideological foundations and permanence of the 1993 report[30] (World Bank, 1993)) and without ever giving themselves the means —and the conviction— to seriously organise it. Once again, we fall back on the classic and long-standing challenges and excesses of targeting[31]. It will be recalled that targeting specific populations benefiting from a public policy instead of a « more universal approach based on law » is one of the classic instruments of the « new public management », says Chelle (2021 : 185) in his analysis of the medical assistance scheme (RAMED) for the indigent in Morocco. Thus, some PBF consultants have even gone so far as to ask countries, without any empirical basis, to impose a quota of 10% on the total number of consultations for the poor, for fear that the latter would abuse the exemption from payment. On examination, the many PBF projects organised with millions of dollars spent will have had very little real impact on the difficult access to care of the populations in sub-Saharan Africa, if any at all on the access to care of the poorest[32]. However, we had warned those in charge of this project for the World Bank in Burkina Faso well in advance on the lack of relevance of their choices —which they heard but never listened to. Will they, like De Ferranti (Rodin & De Ferranti, 2012) and others, make their mea culpa in 20 years? Were these choices part of a stable organisational policy announced long ago (Abbasi, 1999) or an identification of human cognition proposing that:
People identify emotionally with the previously prepared solutions that they have encoded in memory. They tend to become emotionally attached to their current repertoire of encoded solutions, even as the problems they face evolve. As a consequence, reliance on prepared solutions dominates search. (Jones & Thomas, 2013 : 277)
On the other hand, the exemption policies formulated by African states, often based on electoral and clientelist motivations (Olivier de Sardan & Ridde, 2014) have never been supported on such a scale by international organisations, except by the European Union for humanitarian reasons (ECHO). Patients will have benefited very little from the tens of millions of euros spent on the PBF. Health workers will have benefited from bonuses for a few years, or even just a few months, as in Mali[33] and Senegal[34]. The winners may be the national officials, who will also have been able to obtain (often without saying so loudly, as this touches on issues of corruption) significant financial and political incentives, and a leading position within the state apparatus[35]; national and international consultancy firms (the use of these firms is also at the heart of the NPM instruments (Sturdy et al., 2021), which the COVID-19 pandemic has made it possible to talk about again); and national and international NGOs responsible for monitoring and verification, which have seen a significant increase in their turnover and their technical capital. They have taken advantage of this to develop their —African— expertise and try to sell it on an African scale (Gautier, Coulibaly, et al., 2019) to make the PBF model travel better (Olivier de Sardan et al., 2017) or to obtain positions in the senior administration of their state, at the WHO or the World Bank. It is well known that under the leadership of Gro Harlem Brundtland from 1998 to 2003, many economists and authors of the 1993 World Bank report were recruited by the WHO, thus making ideas, vocabulary and people travel. It will be remembered that the few studies published on the cost-effectiveness of PBF have shown how this solution was neither efficient nor even profitable (Antony et al., 2017; Turcotte-Tremblay et al., 2016), as the costs of monitoring and control are so disproportionate for organising payments to providers. For example, in Benin, in the PBF model promoted by the World Bank, for every dollar paid to care providers, $0.50 was used to verify the achievement of the results. This is a far cry from the advice given by the World Bank in 1993 that « Governments have a responsibility to spend well, to get « value for money, » whenever they devote public resources to health » (World Bank, 1993 : 53). Moreover, the numerous studies carried out on the subject have never been made public by the World Bank (for example in Cameroon on its costs or in Benin on the absence of its effectiveness). We recognise the strategic role of knowledge dissemination and the power linked to its control in the context of global governance (Fillol & Ridde, 2020; Gautier & Ridde, 2018).
While waiting for the results of strategic purchasing reforms, this book seems to me to be a demonstration of the recurrence of technical solutions borrowing instruments linked to the ideology of NPM and the financialisation of health. We are at the heart of the mobilisation of path dependency concepts where the choices of the future are guided by the policies of the past (Sabatier & Weible, 2014) instrument autonomy (Veselý, 2021) the problematisation of access to care in a post-structural perspective (Gautier, De Allegri, et al., 2019) end of the story, the losers are always the same: the poor populations who cannot afford to pay for their access to care. This is not a demagogic or populist statement, nor is it a simplistic or radical[36] view of who is to blame; the bad guys in the North and the good guys in the South. Yet, decision-makers in ministries of health and finance in sub-Saharan Africa are aware of these realities and have close (or distant) family members who face ongoing catastrophic expenses. These officials, even when they are at the very top of the hierarchy and can be evacuated to Europe for treatment (the COVID-19 pandemic has once again exposed these privileges!), suffer from daily phone calls to pay for the care of their relatives. The health workers who have to apply the policies of exemption from paying for care (Ridde et al., 2018) are well aware that this solution is relevant. These exemption policies are criticised —with good reason in particular for the delays in the reimbursement process to health facilities that must provide care free of charge. But, those in charge of finance in African ministries are well aware that these exemptions will only be useful if they send budgets in time and in sufficient quantity to compensate them, and allow the health centre to continue to buy medicines (Olivier de Sardan & Ridde, 2014). Experts from both the North and the South are familiar with all these challenges, even if one can imagine that they have somewhat forgotten their youthful field experiences as Peace Corps or students (they often did their fieldwork in these countries or on these subjects). One can also hope that they read the myriad of scientific articles that show that their solutions borrowed from the NPM (direct payment, mutuals, PBF) do not work, either empirically or theoretically (Paul et al., 2021), especially in sub-Saharan African contexts where political power and governance are sometimes weak. Not all countries are like Rwanda[37], which can impose the shift from voluntary to compulsory contributions (which very few people in West Africa know about) for health insurance on their population (whose model dimensions, forgetting the coercive aspects, have been strategically selected (Gautier & Ridde, 2018). Falisse (2019 : 90), returning to the origin of the concept, « the travelling model » proposed by Rottenburg, tells us that « there will always be a form of translation, resistance and acculturation to the model ». Mali, for its part, tried to introduce a compulsory contribution for its civil servants, but officials very quickly backed down in the face of categorical refusals, even though it was finally possible a few years later (Touré & Ridde, 2020). Indeed, trust in the health system as a whole is one of the key mechanisms for the success of fee exemption policies in Africa (Robert et al., 2017) and health reforms in general (Gilson, 2003). History has long taught us that a health system is beyond care. It is a social system where ideas and values are central to its effectiveness (Whyle & Olivier, 2020). Financial incentives, therefore, have only a minimal role in these processes. More than 15 years ago, I already asked the question in response to a biased synthesis published by a World Bank team on the PBF « Building trust or buying results? » (Ridde, 2005).
It is not surprising that a systematic review of PBF-type interventions in 36 low- and middle-income countries recently concluded that « the key mechanisms by which payment for performance can work were not clearly linked to the financial incentive component » (Singh et al., 2021). Why was so much energy and money spent on a solution anchored in the NPM that everyone must have known beforehand would not work? Why did this PBF instrument follow the same blind process as direct payment pilot projects with controlled and unreal conditions; unscientific evaluations focusing on efficiency to the detriment of processes and relevance, and/or with major[38] conflicts of interest, scaling up without rigorous evaluation or taking into account their results, partial or complete failures and then finally, discursive quarantine (direct payment), semantic evolution to keep a low profile (PBF vs. strategic purchase) or disappearance from the debate as in Benin? Perhaps we can find the answer in the analysis proposed by Abimbola (2020 : 11) on the use of experimental methods to evaluate the PBF :
Who is the audience of these randomised controlled trials? The foreign gaze? It is perhaps an easier way to convince funders and unsuspecting, distant, governments who will accept the result as unthinkingly as its cliché deployment by policy entrepreneurs.
Silencing the central issue: public funding
It is well known that pursuing these minimalist solutions does not address the real problem of health systems which is public financing. Indeed, the proportion of health expenditure borne directly by households is still enormous in Africa (Table 1, last column). In 1978, a WHO study group already said « The most obvious solution is to increase government financing » (WHO Study group, 1978 : 21). It is also known that the (former and) current fragmentation of health system financing (Fillol et al., 2020) is not conducive to UHC, nor is the turf war (cover design of the book) between solutions supported by different international donors in a context where some financially dependent governments do not have strong leadership on solutions (Brinkerhoff & Brinkerhoff, 2013; Gautier & Ridde, 2017). Questions of power and ideas (supra) are often at the heart of these issues, influencing the choice of policy instruments, whether it is public policy in general (Béland, 2010) or payment exemption policies in Africa for example (Béland & Ridde, 2016). Let us take two examples to illustrate these external influences in the choice of solutions (Box 1).
|
In Benin, two different models of PBF have been in place for several years. Four international donors (the World Bank, the Global Fund and Gavi on the one hand, and the Belgian cooperation agency (Enabel) on the other) fought for years to promote their approach with projects, expertise and budgets; a battle that led to the national scaling up of PBF (one of the few cases in West Africa). Evaluations, including one by a Senegalese World Bank consultant, showed that the World Bank model was ineffective and inefficient. Gavi and the Global Fund decided to commission a new evaluation, this time by a Belgian researcher known for his ideas in favour of the PBF instrument and a shareholder in a firm selling data management services to PBF countries. However, the results were inconclusive. Most of the evaluation reports concluding that the PBF model supported by the World Bank was ineffective and inefficient were never published. Several joint missions have tried to find a compromise between donors and national actors. However, this was never possible due to turf battles, ideologies and power struggles (Paul, Lamine Dramé, et al., 2018). Eventually, donors all withdrew, sometimes even before the budgetary deadlines, and the PBF has now completely disappeared from the country, not without being considered a notorious failure. In Senegal, the continuation of the « financial protection » component of the UHC was first proposed through the extension of community-based health insurance in all the country’s communes. This solution was largely pushed by an American consultancy firm (Abt Associates) financed by the American cooperation (USAID). While one may question the expertise of this North American country regarding community mutuals[39], one must remember the historical influence of this firm in the 1980s on the deployment of direct payment in Africa (Lee & Goodman, 2002). This firm was also at the heart of organising the national health conference in 2013[40] with, in particular, the presence of a Senegalese economist who had participated in the development of mutual insurance in Rwanda (again!), and under the leadership of people very close to the presidential power (including an anthropologist who would later become director of the National Agency for Universal Health Coverage in 2015). ENABEL then proposed a different model, focusing on departmental pooling and professionalisation (Bossyns et al., 2018). But this proposal met with resistance that delayed the start of the project by several years and limited it to only two departments. The results of this new proposal are now so convincing, even after the Belgian-funded project was stopped (Mbow et al., 2020), that the state has decided to learn from it. The state is beginning to test some form of professionalisation in other departments of the country, and a cooperation from Luxembourg is supporting the transfer of the model to other departments. But some years have certainly been lost. |
These two examples show that the power issues are often located around the choice of some very specific solutions but never really refer to the fundamental question, that of national public funding. Yet, if we return to the question of funding sources, we know that the more they are pooled into a single common public basket (pooled financing), the more countries move towards UHC (Lozano et al., 2020). As long as sub-Saharan states do not decide to devote a larger share of their budget to the health sector (Table 1), organise mutual insurance schemes with voluntary membership or set up a fully externally financed PBF, this will not have a strong impact on access to care and health system strengthening. The advocacy group of former world leaders (The Elders) has stated the following truism: « If there is one lesson the world has learned, it is that UHC can only be achieved through public financing » (Yates, 2021). However, the issue is not discussed in public arenas, beyond reports and speeches (WHO, 2020a).
For example, in recent years the WHO has launched a series of studies on what it calls innovative financing. The needs are indeed enormous in this respect as revealed by a very recent systematic review of funding strategies for the UHC: « It is evident from the review that innovative health financing strategies in SSA are needed » (Ifeagwu et al., 2021 : 1). However, they remain sadly superficial (as were the 1978 proposals (WHO Study group, 1978)) and seek to find derisory sums by proposing to tax telephone communications, tobacco or even airline tickets. For example, in Mali in 2015, participatory workshops were held to select financing mechanisms from a list of 24 proposals made by the consultants. The five selected for in-depth analysis were a tax on alcohol, mining resources, telephone, airline tickets and financial transactions. But the consultants’ conclusions are clear: « The proposal for an additional tax on mining resources seems difficult… Moreover, there is a lack of transparency on the taxes paid by these companies and on the quantities actually extracted. This lack of transparency poses a problem of accountability of decision-makers to their population. The mining sector has enormous potential but requires strong political will to implement a tax » (Traore & Brikci, 2016). In their final calculations and general recommendations to the Government of Mali, the consultants did not retain the possibility of taxing the mining sector and only proposed a tax on airline tickets, alcohol and the telephone sector. They even state that « an additional tax on mining resources … is not feasible in the current economic and political context » (Traore & Brikci, 2016). The Senegalese example also shows that beyond the technical aspects, it is the political will and the fiscal space that is decisive for UHC (Paul et al., 2020). The government of Burkina Faso also lacked determination by ignoring the results of an International Monetary Fund (IMF) study proposing to stop the inefficient hydrocarbon price subsidy in favour of a direct cash transfer programme to the poorest (Kadio et al., 2018). The political and social stakes of this removal of a tax benefiting the least poor had taken precedence over the needs of the « lowly » populations.
For example, most studies of this kind are hampered by the challenge of mobilising the enormous financial potential of the extractive industry, which is booming in West Africa (Ridde et al., 2015). Changing mining codes in favour of UHC appears to be difficult, and international mining companies are doing their utmost to further reduce the capacity of states to govern this lucrative sector. The ideological perspective just described in the health sector is also present in the extractive sector where orthodox economists are calling for market liberalisation and tax avoidance by private companies. The World Bank’s Doing Business[41] indicators for ranking countries according to their business-friendly regulations are a good example of this approach. In Mali, the recent 2019 mining code —which is not retroactive— has limited the reduced 25% corporate tax rate to three years from 15 years in the previous 2012 code (Zitti & Diawara, 2021). Moreover, almost 20% of the Malian state’s current revenue in 2017 came from the extractive sector. However, while the country exported CFAF 1024 billion in mineral resources in 2016, only CFAF 241 billion in revenues were found. The Extractive Industries Transparency Initiative committee stated that « some 20 companies exported gold without holding a mining licence or being listed in the mining register in 2016 » (Zitti & Diawara, 2021). While the mining industry has to make social payments, they represented only 0.6% of revenues, not to mention the challenges of tracking them. We could multiply the examples in the region and elsewhere in the world, of course, with Western industries at the centre of the issues. The figures can quickly become staggering when it comes to tax evasion/avoidance and corruption (Coderre, 2019). For example, it is estimated that between 2000 and 2010, sub-Saharan Africa lost $50 billion in illicit capital, 56% of which came from the extractive sector. Worse still « according to the Global Financial Integrity, the continent bears the most disproportionate burden of unrecorded cross-border financial outflows as a percentage of gross domestic product (GDP), representing approximately 8.6 per cent of GDP » (UN ECA, 2017). In Malawi, the tax benefits granted to an Australian mining company between 2009 and 2014 amounted to $43 million, or the annual salary of 17,000 nurses (ActionAid, 2015). It will be recalled that the cost of an essential health package worldwide was estimated at $34 per person in 2001, then $44 by the WHO in 2009 and $60 in 2015 (OMS, 2015). These figures hide disparities between countries, but they give an idea of the scale of the needs and the capacity to meet them by mobilising public funds. However, once again we find our friend the NPM, and it is essentially the criteria of efficiency (which the 1993 World Bank report had put forward following, in particular, the WHO in 1978 (WHO Study group, 1978) and effectiveness that take priority in the choice of the content of these countries for the type of interventions selected, with the issues of equity or the needs of the populations largely forgotten in these studies (Hayati et al., 2018).
Conclusion
This collective work aims to share in French the most recent scientific knowledge on contemporary strategies to move towards UHC in sub-Saharan Africa and in particular the reforms linked to its financing. The introduction proposes a global reflection based on the chapters, which all show, according to the countries and strategies, the permanence of the mobilisation of political instruments largely inspired by the New Public Management whose challenges are widely known and whose effectiveness is very relative. However, these instruments persist and the ideas of those who try to promote them, sometimes even to impose them in a context of dependence on international aid, show how much power issues are at the heart of health system reforms. However, there is nothing new in this area (Erasmus & Gilson, 2008) even if it must be constantly recalled (Topp, 2020). More than just a technical issue, the transformation of health systems, and in particular that of their financing methods, is a major political issue where values and ideologies are the sources of proposed solutions. As we have seen, they sometimes correspond more to the thesis of a handful of experts (from both the North and the South) than to the evidence and the state of scientific knowledge. But if public policy instruments were based on science, this would be known (Fillol et al., 2020). Thus, this group of authors has carried out rigorous empirical studies and mobilised theories and conceptual frameworks relevant to their contexts to share scientific knowledge to better understand the emergence, implementation, effects and prospects of these reforms in a few sub-Saharan African countries over the past decade. Much remains to be done to bring these countries closer to the UHC ideal, but we hope that the analyses offered (without direct payment) in this book will be able to enlighten reflections and let us dream a little, decisions.
Références
Abbasi, K. (1999). The World Bank and world health: Healthcare strategy. BMJ, 318(7188), 933‑936. https://doi.org/10.1136/bmj.318.7188.933
Abiiro, G. A., & De Allegri, M. (2015). Universal health coverage from multiple perspectives: A synthesis of conceptual literature and global debates. BMC International Health and Human Rights, 15(17). https://doi.org/10.1186/s12914-015-0056-9
Abimbola, S. (2020). Evidence as cliché: Using trials to tamper with governance. CODESRIA Bulletin, 4, 9‑15.
ActionAid. (2015, 17 juin). An Extractive Affair. https://actionaid.org/publications/2015/extractive-affair
Amnesty International. (2009, 31 décembre). Giving life, risking death. Maternal mortality in Burkina Faso. Amnesty International Publications. https://www.amnesty.org/en/documents/afr60/001/2009/en/
Amri, M. M., Jessiman-Perreault, G., Siddiqi, A., O’Campo, P., Enright, T. & Di Ruggiero, E. (2021). Scoping review of the World Health Organization’s underlying equity discourses : Apparent ambiguities, inadequacy, and contradictions. International Journal for Equity in Health, 20(70). https://doi.org/10.1186/s12939-021-01400-x
Antony, M., Bertone, M. P. & Barthes, O. (2017). Exploring implementation practices in results-based financing: The case of the verification in Benin. BMC Health Services Research, 17(204). https://doi.org/10.1186/s12913-017-2148-9
Balique, H., Ouattara, O. & Ag Iknane, A. (2001). Dix ans d’expérience des centres de santé communautaire au Mali. Santé Publique, 13(1), 35‑48.
Batifoulier, P. (2013). Faire payer le patient : Une politique absurde. Revue du MAUSS, 41(1), 77-92. https://doi.org/10.3917/rdm.041.0077
Belaid, L., Cloos, P. & Ridde, V. (2017). Mobiliser des représentations ethnoculturelles pour expliquer les disparités d’accès aux soins de santé au Burkina Faso. Canadian Journal of Public Health, 108, 56-61. https://doi.org/10.17269/cjph.108.5628
Béland, D. & Cox, R. H. (dir.). (2011). Ideas and politics in social science research. Oxford University Press.
Béland, D. & Ridde, V. (2016). Ideas and policy implementation : Understanding the resistance against free health care in Africa. Global Health Governance, 10(3), 9‑23.
Béland, D. (2010). The idea of power and the role of ideas. Political Studies Review, 8(2), 145‑154. https://doi.org/10.1111/j.1478-9302.2009.00199.x
Bodson, O. (2021). Le financement basé sur les résultats au Bénin et au Sénégal : Un levier pérenne de changement de pratiques des agents de santé? [Thèse de doctorat en sciences politiques et sociales]. Université de Liège.
Boidin, B. (2014). La santé, bien public mondial ou bien marchand : Réflexions à partir des expériences africaines. Presses universitaires du Septentrion.
Bossyns, P., Ladrière, F. & Ridde, V. (2018). Une assurance maladie à grande échelle pour le secteur informel en Afrique subsaharienne. Six ans d’expérience au Sénégal rural 2012 – 2017 (Studies in Health Services Organisation&Policy, 34, 2018). ITGPress. https://www.itg.be/files/docs/shsop/shsop34.pdf
Brinkerhoff, D. W. & Brinkerhoff, J. M. (2013). Development management and policy implementation. Relevance beyond the global South. Dans E. Araral, S. Fritzen, M. Howlett, M. Ramesh, & X. Wu (dir.), Routledge handbook of public policy (274‑383). Routledge.
Chelle, E. (2021). Quel droit à la santé pour les populations pauvres au Maroc? La longue gestation du Régime d’assistance médicale (RAMED). Dans M. Borgetto, M. Chauvière & W. Tamzini (dir.), La protection sociale au Maghreb et en France. Regards croisés (181‑192). Mare & Martin.
Coderre, M. (2019). Maximisation et mobilisation des revenus du secteur minier en Afrique subsaharienne : Quelles stratégies pour favoriser le développement? [Rapport, Revue de littérature (2)]. Accès à la santé, ressources minières et politiques publiques en Afrique subsaharienne, Université du Québec à Montréal.
Diagne, A. & Sylla F. (2021). Soutenabilité budgétaire du Programme national de couverture maladie universelle du Sénégal (Rapport provisoire). CRES.
D’Adesky, J. (2017). Subalternité. Dans Anthropen. https://doi.org/10.17184/eac.anthropen.056
De Ferranti, D. (1985). Paying for health services in developping countries [World Bank Staff Working Papers]. World Bank.
De Walque, D., Robyn, P. J., Saidou, H., Sorgho, G. & Steenland, M. (2017). Looking into the performance-based financing black box: Evidence from an impact evaluation in the health Sector in Cameroon [Policy Research Working Paper, (8162)]. World Bank. https://openknowledge.worldbank.org/handle/10986/27969
Deville, C., Hane, F., Ridde, V. & Touré, L. (2018). La Couverture universelle en santé au Sahel : La situation au Mali et au Sénégal en 2018 (Working Papers, (40), p. 38). CEPED.
Erasmus, E. & Gilson, L. (2008). How to start thinking about investigating power in the organizational settings of policy implementation. Health Policy & Planning, 23(5), 361‑368.
Evans, R., Barer, M. & Stoddart, G. (1993). User fees for health care: Why a bad idea keeps coming back (Or, what’s health got to do with it?). Canadian Journal on Aging ⁄ Revue Canadienne Du Vieillissement, 14, 360-390.
Falisse, J. B. (2019). Au-delà du modèle voyageur? Usage stratégique et hybridation du financement basé sur la performance (FBP) dans la santé au Burundi. Politique africaine, 156, 83‑100.
Fassin, D. (2000). Comment faire de la santé publique avec des mots. Une rhétorique à l’oeuvre. Ruptures, 7(1), 58‑78.
Fillol, A., Kadio, K. & Gautier, L. (2020). L’utilisation des connaissances pour informer des politiques publiques : D’une prescription technocratique internationale à la réalité politique des terrains. Revue française des affaires sociales, 4, 103‑127. https://doi.org/10.3917/rfas.204.0103
Fillol, A. & Ridde, V. (2020). Gouvernance globale et utilisation des connaissances pour l’action: Revue francophone de recherche sur le transfert et l’utilisation des connaissances, 4(2). https://doi.org/10.18166/tuc.2020.4.2.15
Gage, A. & Bauhoff, S. (2021). The effects of performance-based financing on neonatal health outcomes in Burundi, Lesotho, Senegal, Zambia and Zimbabwe. Health Policy & Planning, 36(3), 332-340. https://doi.org/10.1093/heapol/czaa191
Gaudillière, J.-P., Beaudevin, C., Gradmann, C., Lovell, A. & Pordié, L. (2020). Global health and the new world order historical and anthropological approaches to a changing regime of governance. Manchester University Press.
Gautier, L., Coulibaly, A., De Allegri, M. & Ridde, V. (2019). From Amsterdam to Bamako: A qualitative case study on diffusion entrepreneurs’ contribution to performance-based financing propagation in Mali. Health Policy & Planning, 34(9), 656-666. https://doi.org/10.1093/heapol/czz087
Gautier, L., De Allegri, M. & Ridde, V. (2019). How is the discourse of performance-based financing shaped at the global level? A poststructural analysis. Globalization and Health, 15(1). https://doi.org/10.1186/s12992-018-0443-9
Gautier, L. & Ridde, V. (2017). Health financing policies in Sub-Saharan Africa: Government ownership or donors’ influence? A scoping review of policymaking processes. Global Health Research and Policy, 2(23).
Gautier, L. & Ridde, V. (2018). Did the learning agenda of the World Bank-administrated Health Results Innovation Trust Fund shape politicised evidence on performance-based financing? A documentary analysis. Sociedade e Cultura, 21(2). https://doi.org/10.5216/sec.v21i2.56310
Gautier, L., Tosun, J., De Allegri, M. & Ridde, V. (2018). How do diffusion entrepreneurs spread policies? Insights from performance-based financing in Sub-Saharan Africa. World Development, 110, 160‑175. https://doi.org/10.1016/j.worlddev.2018.05.032
Gélinas, J. B. (2000). La globalisation du monde. Laissez faire ou faire? Écosociété.
Ghanbari, M. K., Behzadifar, M., Doshmangir, L., Martini, M., Bakhtiari, A., Alikhani, M. & Bragazzi, N. L. (2021). Mapping research trends of universal health coverage from 1990 to 2019: Bibliometric analysis. JMIR Public Health and Surveillance, 7(1). https://doi.org/10.2196/24569
Gilson, L. (2003). Trust and the development of health care as a social institution. Social science & medicine, 56(7), 1453‑1468.
Gilson, L. (dir.) (2012). Recherche sur les politiques et les systèmes de santé santé. Manuel de Méthodologie. Version abrégée. Alliance pour la recherche sur les politiques et les systèmes de santé, Organisation mondiale de la Santé. https://www.who.int/alliance-hpsr/resources/alliancehpsr_readerabridgedfrench.pdf?ua=1
Gilson, L., Kalyalya, D., Kuchler, F., Lake, S., Organa, H. & Ouendo, M. (2000). The equity impacts of community financing activities in three African countries. International Journal of Health Planning and Management, 15(4), 291-317. doi:10.1002/hpm.599.
Handayani, K., Sijbranda, T. C., Westenberg, M. A., Rossell, N., Sitaresmi, M. N., Kaspers, G. J. & Mostert, S. (2020). Global problem of hospital detention practices. International Journal of Health Policy and Management, 9(8), 319-326. https://doi.org/10.15171/ijhpm.2020.10
Hayati, R., Bastani, P., Kabir, M. J., Kavosi, Z., & Sobhani, G. (2018). Scoping literature review on the basic health benefit package and its determinant criteria. Globalization and Health, 14(26). https://doi.org/10.1186/s12992-018-0345-x
Howlett, M. P. (2011). Designing public policies: Principles and instruments. Routledge.
Ifeagwu, S. C., Yang, J. C., Parkes-Ratanshi, R. & Brayne, C. (2021). Health financing for universal health coverage in Sub-Saharan Africa: A systematic review. Global Health Research and Policy, 6(8). https://doi.org/10.1186/s41256-021-00190-7
Jaffré, Y. & Olivier de Sardan, J.-P. (dir.) (2003). Une médecine inhospitalière. Les difficiles relations entre soignants et soignés dans cinq capitales d’Afrique de l’Ouest. APAD, Karthala.
Jones, B. D. & Thomas, H. F. (2013). Bounded rationality and public policy decision-making. Dans E. Araral, S. Fritzen, M. Howlett, M. Ramesh & X. Wu (dir.), Routledge handbook of public policy (273‑286). Routledge.
Jones, C., Gautier, L. & Ridde, V. (2021). A scoping review of theories and conceptual frameworks used to analyse health financing policy processes in sub-Saharan Africa. Health Policy & Planning, 1‑17 (sous presse). https://doi.org/10.1093/heapol/czaa173
Kadio, K., Dagenais, C. & Ridde, V. (2018). Politique nationale de protection sociale du Burkina Faso : Contexte d’émergence et stratégies des acteurs. Revue française des affaires sociales, (1), 63‑84.
Kaul, M. (1997). The New Public Administration: Management innovations in government. Public Administration and Development, 17(1), 13‑26. https://doi.org/10.1002/(SICI)1099-162X(199702)17:1<13::AID-PAD909>3.0.CO;2-V
Klasa, K., Greer, S. L. & van Ginneken, E. (2018). Strategic purchasing in practice: Comparing ten european countries. Health Policy, 122(5), 457‑472. https://doi.org/10.1016/j.healthpol.2018.01.014
Koulidiati J. L., De Allegri M., Lohmann J. et al. (2021). Impact of performance-based financing on effective coverage for curative child health services in Burkina Faso: Evidence from a quasi-experimental design. Tropical Medicine & International Health. doi: 10.1111/tmi.13596.
Kumar, S. & Watkins, R. (2017). The art of designing and implementing study tours: A guide based on the art of knowledge exchange methodology. World Bank. https://openknowledge.worldbank.org/handle/10986/28405
Lee, K. & Goodman, H. (2002). Global policy networks: The propagation of health care financing reform since the 1980s. Dans K. Lee, K. Buse & S. Fustukian (dir.), Health policy in a globalising world (97‑199). Cambridge University Press.
Lipsky, M. (2010). Street-level bureaucracy. Dilemmas of the individual in public services. Russel Sage Foundation.
Louart, S., Bonnet, E. & Ridde, V. (2020). Is patient navigation a solution to the problem of « leaving no one behind »? A scoping review of evidence from low-income countries. Health Policy & Planning, 36(1), 101-116. https://doi.org/10.1093/heapol/czaa093
Lozano, R., Fullman, N., Mumford, J. E. et al. (2020). Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1250‑1284. https://doi.org/10.1016/S0140-6736(20)30750-9
Martin, B. (2015). L’adieu à l’humanitaire? Les ONG au défi de l’offensive néolibérale. Éditions Charles Léopold Mayer.
Mathauer, I., Mathivet, B. & Kutzin, J. (2017). Free health care policies: Opportunities and risks for moving towards UHC. World Health Organization.
Mathauer, I., Dale, E., Jowett, M. & Kutzin, J. (2019). Purchasing health services for universal health coverage: How to make it more strategic? World Health Organization.
Mbow, N. B., Senghor, I. & Ridde, V. (2020). The resilience of two professionalized departmental health insurance units during the COVID-19 pandemic in Senegal. Journal of Global Health, 10(2), 1‑6. https://doi.org/10.7189/jogh.10.020394
McCoy, D., Hall, J. A. & Ridge, M. (2012). A systematic review of the literature for evidence on health facility committees in low- and middle-income countries. Health Policy & Planning, 27(6), 449‑466.
McIsaac, M., Kutzin, J., Dale, E. & Soucat, A. (2018). Results-based financing in health: From evidence to implementation. Bulletin of the World Health Organization, 96(11), 730-730A. https://doi.org/10.2471/BLT.18.222968
Mills, A., Bennett, S., Russell, S. & Attanayake, N. (2001). The challenge of health sector reform: What must governments do? Palgrave.
Mladovsky, P., Ndiaye, P., Ndiaye, A. & Criel, B. (2015). The impact of stakeholder values and power relations on community-based health insurance coverage : Qualitative evidence from three Senegalese case studies. Health Policy & Planning, 30(6), 768‑781. https://doi.org/10.1093/heapol/czu054
Mladovsky, P. (2020). Fragmentation by design: Universal health coverage policies as governmentality in Senegal. Social Science & Medicine, 260(113153). https://doi.org/10.1016/j.socscimed.2020.113153
Mwase, T., Lohmann, J., Hamadou, S., Brenner, S., Somda, S.M.A., Hien, H., Hillebrecht, M. & De Allegri, M. (2020). Can combining performance-based financing with equity measures result in greater equity in utilization of maternal care services? Evidence from Burkina Faso. International Journal of Health Policy and Management. doi:10.34172/ijhpm.2020.121.
Moulin, A.-M. (2021). Guérir en Afrique ou le silence qui parle. Dans A. Desclaux, A. Diarra & S. Musso (dir.), Guérir en Afrique : Promesses et transformations (postface). L’Harmattan, coll. Anthropologies & Médecines.
Olivier de Sardan, J.-P. (2021). La revanche des contextes. Des mésaventures de l’ingéniérie sociale en Afrique et au-delà. Karthala.
Olivier de Sardan, J.-P., Diarra, A. & Moha, M. (2017). Travelling models and the challenge of pragmatic contexts and practical norms: The case of maternal health. Health Research Policy and Systems, 15(60). https://doi.org/10.1186/s12961-017-0213-9
Olivier de Sardan, J.-P. & Ridde, V. (dir.) (2014). Une politique publique de santé et ses contradictions. La gratuité des soins au Burkina Faso, au Mali et au Niger. Karthala.
OMS. (2015). Faire des choix justes pour une couverture sanitaire universelle. Rapport final du Groupe Consultatif de l’OMS sur la Couverture Sanitaire Universelle et Équitable. Organisation mondiale de la Santé; WHO IRIS. https://apps.who.int/iris/handle/10665/185069
Paganini, A. (2004). The Bamako Initiative was not about money. Health Policy and Development, 2(1), 11‑13.
Paul, E., Albert, L., Bisala, B. N. et al. (2018). Performance-based financing in low-income and middle-income countries: Isn’t it time for a rethink? BMJ Global Health, 3(1). https://doi.org/10.1136/bmjgh-2017-000664
Paul, E., Bodson, O. & Ridde, V. (2021). What theories underpin performance-based financing? A scoping review. Journal of Health Organization and Management, 35(3), 344-381. https://doi.org/10.1108/JHOM-04-2020-0161
Paul, E., Brown, G. W., Ensor, T., Ooms, G., van de Pas, R. & Ridde, V. (2020). We shouldn’t count chickens before they hatch: Results-based financing and the challenges of cost-effectiveness analysis. Critical Public Health, 31(3). https://doi.org/10.1080/09581596.2019.1707774
Paul, E., Lamine Dramé, M., Kashala, J.-P., Ekambi Ndema, A., Kounnou, M., Codjovi Aïssan, J. & Gyselinck, K. (2018). Performance-based financing to strengthen the health system in Benin : Challenging the mainstream approach. International Journal of Health Policy and Management, 7(1), 35‑47. https://doi.org/10.15171/ijhpm.2017.42
Paul, E., Ndiaye, Y., Sall, F. L., Fecher, F. & Porignon, D. (2020). An assessment of the core capacities of the Senegalese health system to deliver Universal Health Coverage. Health Policy OPEN, 1(100012). https://doi.org/10.1016/j.hpopen.2020.100012
Paul, E., Sieleunou, I. & Ridde, V. (2018, mars). Comment utiliser l’expérience de financement basé sur les résultats (FBR) pour rendre l’achat des services de santé plus stratégique au Bénin? Cahiers Réalisme, (15). http://www.equitesante.org/wp-content/uploads/2018/03/Numero-15-Mars-2018.pdf
Pigeon-Gagné, É. (2021). « même s’ils sont guéris, on dit qu’ils sont des fous » : Une étude ethnographique sur la stigmatisation des troubles de santé mentale dans la ville de Bobo-dioulasso [Thèse de doctorat en psychologie]. Université du Québec à Montréal.
Prince, R. (2017). Universal health coverage in the Global South : New models of healthcare and their implications for citizenship, solidarity, and the public good. Michael, 14(2), 153‑172.
Renault, E. (2008). Le néolibéralisme et sa pensée critique. Lignes, 1(25), 102‑119. https://www.cairn.info/revue-lignes-2008-1-page-102.html
Ridde, V. (2005). Performance-based partnership agreements for the reconstruction of the health system in Afghanistan. Development in Practice, 15(1), 4‑15.
Ridde, V. (2011). Is the Bamako Initiative still relevant for West African health systems? International Journal of Health Services, 41(1), 175‑184.
Ridde, V. (2015). From institutionalization of user fees to their abolition in West Africa: A story of pilot projects and public policies. BMC Health Services Research, 15(3), 1‑11. https://doi.org/10.1186/1472-6963-15-S3-S6
Ridde, V. & Jacob, J. P. (2013). Les indigents et les politiques de santé en Afrique. Expériences et enjeux conceptuels. Academia, L’Harmattan.
Ridde, V. (2005). Building trust or buying results? The Lancet, 366(9498). https://doi.org/10.1016/S0140-6736(05)67689-1
Ridde, V., Aho, J., Ndao, E. M., Benoit, M., Hanley, J., Lagrange, S., Fillol, A., Raynault, M.-F. & Cloos, P. (2020). Unmet healthcare needs among migrants without medical insurance in Montreal, Canada. Global Public Health, 15(11) 1‑14. https://doi.org/10.1080/17441692.2020.1771396
Ridde, V., Bonnet, E., Kadio, K., Louart, S. & De Allegri, M. (2019). Demographics in the service of universal health coverage: Examples in West Africa. Humanitarian Alternatives, 12, 33‑48.
Ridde, V., Campbell, B. & Martel, A. (2015). Mining revenue and access to health care in Africa: Could the revenue drawn from well-managed mining sectors finance exemption from payment for health? Development in Practice, 25(6), 909‑918. https://doi.org/10.1080/09614524.2015.1062470
Ridde, V. & Fillol, A. (2021). La santé mondiale. Dictionnaire en ligne Anthropen https://revues.ulaval.ca/ojs/index.php/anthropen
Ridde, V., Leppert, G., Hien, H., Robyn, P. J. & De Allegri, M. (2018). Street-level workers’ inadequate knowledge and application of exemption policies in Burkina Faso jeopardize the achievement of universal health coverage: Evidence from a cross-sectional survey. International Journal for Equity in Health, 17(5). https://doi.org/10.1186/s12939-017-0717-5
Ridde, V. & Ouattara, F. (2015). Des idées reçues en santé mondiale. Presses de l’Université de Montréal; Presses de l’École des Hautes Études en Santé Publique.
Ridde, V., Pérez, D. & Robert, E. (2020). Using implementation science theories and frameworks in global health. BMJ Global Health, 5(4). https://doi.org/10.1136/bmjgh-2019-002269
Ridde, V., Queuille, L. & Ndour, M. (2014). Nine misconceptions about free healthcare in sub-Saharan Africa. Development Studies Research, 1(1), 54‑63. https://doi.org/10.1080/21665095.2014.925785
Robert, E. & Ridde, V. (2013). Global health actors no longer in favor of user fees: A documentary study. Globalization and health, 9(29). https://doi.org/10.1186/1744-8603-9-29
Robert, E. & Ridde, V. (2016). Quatre principes de recherche pour comprendre les défis des systèmes de santé des pays à faible et moyen revenu. Canadian Journal of Public Health, 107, e362–e365. https://doi.org/10.17269/cjph.107.5533
Robert, E., Ridde, V., Rajan, D., Sam, O., Dravé, M. & Porignon, D. (2019). Realist evaluation of the role of the Universal Health Coverage Partnership in strengthening policy dialogue for health planning and financing: A protocol. BMJ Open, 9(1). https://doi.org/10.1136/bmjopen-2018-022345
Robert, E., Samb, O. M., Marchal, B. & Ridde, V. (2017). Building a middle-range theory of free public healthcare seeking in sub-Saharan Africa: A realist review. Health Policy & Planning, 32(7), 1002‑1014. https://doi.org/10.1093/heapol/czx035
Rodin, J. & De Ferranti, D. (2012). Universal health coverage: The third global health transition? The Lancet, 380, 861‑862.
Rose, R. (2005). Learning from comparative public policy. A practical guide. Routledge.
Roth, C. (2012). The Nivaquine children’ – the intergenerational transfer of knowledge about old age and gender in urban Burkina Faso. Dans W. Röder & K. de Jong (dir.), Alter(n) anders denken. Kulturelle und biologische Perspektiven. Böhlau Verlag.
Sabatier, P. A. & Weible, C. M. (dir.) (2014). Theories of the policy process (Third edition). Westview Press, a member of the Persus Books Group.
Singh, N. S., Kovacs, R. J., Cassidy, R., Kristensen, S. R., Borghi, J. & Brown, G. W. (2021). A realist review to assess for whom, under what conditions and how pay for performance programmes work in low- and middle-income countries. Social Science & Medicine, 270. https://doi.org/10.1016/j.socscimed.2020.113624
Soors, W., Dkhimi, F. & Criel, B. (2013). Lack of access to health care for African indigents: A social exclusion perspective. International Journal for Equity in Health, 12(91). https://doi.org/10.1186/1475-9276-12-91
Soucat, A. & Kickbusch, I. (2020). Global common goods for health : Towards a new framework for global financing. Global Policy, 11(5), 628‑635. https://doi.org/10.1111/1758-5899.12875
Sturdy, A. J., Kirkpatrick, I., Reguera, N., Blanco‐Oliver, A. & Veronesi, G. (2021). The management consultancy effect: Demand inflation and its consequences in the sourcing of external knowledge. Public Administration. https://doi.org/10.1111/padm.12712
The Global Campaign for the Health Millennium Development Goals. (2009). Leading by example – Protecting the most vulnerable during the economic crisis [Rapport]. Office of the Prime Minister of Norway. https://reliefweb.int/report/world/leading-example-protecting-most-vulnerable-during-economic-crisis-global-campaign
Thiongane, O. (2021) En Afrique, la notion d’hésitation vaccinale est un modèle voyageur. The Conversation. https://theconversation.com/en-afrique-la-notion-dhesitation-vaccinale-est-un-modele-voyageur-158035
Topp, S. M. (2020). Power and politics: The case for linking resilience to health system governance. BMJ Global Health, 5(6). https://doi.org/10.1136/bmjgh-2020-002891
Touré, L. & Ridde, V. (2020). The emergence of the national medical assistance scheme for the poorest in Mali. Global Public Health. https://doi.org/10.1080/17441692.2020.1855459
Traore, M. & Brikci, N. (2016). Le financement de la santé au Mali à travers les sources de financement innovantes [Rapport final]. Oxford Policy Management, OMS, MSAH
Turcotte-Tremblay, A.-M., De Allegri, M., Gali-Gali, I. A. & Ridde, V. (2018). The unintended consequences of combining equity measures with performance-based financing in Burkina Faso. International Journal for Equity in Health, 17(109). https://doi.org/10.1186/s12939-018-0780-6
Turcotte-Tremblay, A.-M., Spagnolo, J., De Allegri, M. & Ridde, V. (2016). Does performance-based financing increase value for money in low- and middle- income countries? A systematic review. Health Economics Review, 6(30). https://doi.org/10.1186/s13561-016-0103-9
UN ECA. (2017). Impact of illicit financial flows on domestic resource mobilization : Optimizing revenues from the mineral sector in Africa. United Nations. Economic Commission for Africa. Special Initiatives Division. African Minerals Development Center; African Union Commission.
Van de Poel, E., Flores, G., Ir, P. & O’Donnell, O. (2016). Impact of performance-based financing in a low-resource setting: A decade of experience in Cambodia. Health Economics, 25(6), 688‑705. https://doi.org/10.1002/hec.3219
Veselý, A. (2021). Autonomy of policy instrument attitudes: Concept, theory and evidence. Policy Sciences, 54, 441–455. https://doi.org/10.1007/s11077-021-09416-4
Vuarin, R. (2000). Un système africain de protection sociale au temps de la mondialisation, ou « Venez m’aider à tuer mon lion ». L’Harmattan.
Waelkens, M.-P., Werner, S. & Bart, C. (2017). Community health insurance in low- and middle-income countries. Dans International Encyclopedia of Public Health (82‑92). Elsevier. https://doi.org/10.1016/B978-0-12-803678-5.00082-5
WHO. (2020a). Global spending on health 2020 : Weathering the storm. World Health Organization.
WHO. (2020b). Strategy Report: Engaging the private health service delivery sector through governance in mixed health systems. World Health Organization.
WHO Study group. (1978). Financing of health services [Technica report series 625]. World Health Organization.
Whyle, E. & Olivier, J. (2020). Social values and health systems in health policy and systems research: A mixed-method systematic review and evidence map. Health Policy & Planning, 35(6), 735‑751. https://doi.org/10.1093/heapol/czaa038
World Bank. (1993). World Development Report 1993: Investing in Health. Oxford University Press.
Yates, R. (2021). Pooled public financing is the route to universal health coverage. The Lancet, 397(10273), 472. https://doi.org/10.1016/S0140-6736(21)00225-7
Zeng, W., Shepard, D. S., Nguyen, H., Chansa, C., Das, A. K., Qamruddin, J. & Friedman, J. (2018). Cost–effectiveness of results-based financing, Zambia: A cluster randomized trial. Bulletin of the World Health Organization, 96(11), 760‑771. https://doi.org/10.2471/BLT.17.207100
Zitti, T. & Diawara, A. (2021). Défis et opportunités du secteur minier malien à couvrir les services sociaux : Cas de la couverture sanitaire universelle [Rapport]. Accès à la santé, ressources minières et politiques publiques en Afrique subsaharienne.
- I would like to thank Oriane Bodson, Sarah Louart, Philippe Lavigne Delville and David Reubi for their very helpful comments on an earlier version of this introduction. Thanks a lot, to Treasure Udechukwu and Kalamaushika Vikna Theyagarajan for the English editing support. ↵
- https://www.who.int/features/qa/universal_health_coverage/fr/ ↵
- See most chapters in this book ↵
- See the chapter by Gautier et al. ↵
- See the chapter by Ridde and Yaméogo ↵
- See the chapter by Dagenais et al. ↵
- See the chapter by Louart et al. ↵
- See the chapter by Beaugé et al. ↵
- Thanks to Sofia Meister for putting me back on the path of Gramsci, which I had encountered long ago, and for opening my eyes to the conceptual perspectives that we will try to mobilise through a research project on access to healthcare in Haiti and Bangladesh https://www.climhb.org ↵
- For the index of service coverage in 2017 : Average coverage of essential services based on interventions that include reproductive, maternal, newborn and child health, infectious diseases, non-communicable diseases and capacity and access to services. ↵
- See the chapter by Chemouni ↵
- See the chapter by Ridde et al. ↵
- See the chapters by Ridde and Yaméogo, and Nguyen et al. ↵
- The concept has not yet been fully elucidated, but it essentially involves combining incentives with the financing of health facilities and health professionals to optimise use of resources. It is presented by its advocates as a tool for improving the efficiency of resource use. On processes, the approach "consists mainly of linking health financing to information on (i) the health needs of the population and (ii) the performance of health providers, based on active and evidence-based engagement" (Paul et al., 2018 : 5). ↵
- In Mali, a study tour to Rwanda (again) in 2009 enabled those in charge to understand the importance of mutualisation, no longer at village level but at communal level. It is likely that 2022 (following the PADS2 project financed by the AFD) will see a new change of scale with the organisation of mutuals at the district (cercle) level and compulsory membership. ↵
- On the history of contracting: "In the Middle Ages, documents prove that healing could be the subject of a contract between the practitioner and his client, and reimbursement of fees was even provided for in case of failure" (Moulin, 2021 : 343). ↵
- See chapter by Ridde et al. ↵
- It will be recalled that in 1978 the WHO already stated " The financial contributions of the local people give them both the right and the incentive to participate in the running of the program. Such participation is an important base upon which to build health awareness in its widest sense and generate those changes in personal behaviour which can contribute to raising health standards" (WHO Study group, 1978 : 28-29) ↵
- See the chapter by Ridde and Yaméogo ↵
- See Dagenais' chapter ↵
- Anne-Marie Moulin (2021 : 341) explains that "The saints, known as anargyroi, operated without money, for free. Fees, which appeared scandalous in a profession related to the sacred, were the subject of a debate that spanned over centuries". ↵
- See the chapters by Ridde et al., and Chemouni ↵
- Their frontline workers are often unaware of their position in favour of abolishing direct payments (The Global Campaign for the Health Millennium Development Goals, 2009) ↵
- In Mali, to disseminate the idea of PBF, "results-based dinners" at the Hotel Nord-Sud in Bamako were organised from the 2010s onwards. Facilitated by the Dutch expert and his Malian colleagues" (Fillol et al., 2020 : 118). The World Bank has even produced a manual to make influence trips or other study tours more effective (Kumar & Watkins, 2017) ↵
- On the financialisation of NGOs and humanitarianism, see (Martin, 2015) ↵
- It postulates that economic agents are rational and focused on the utility of their choices, that the market economy is superior, that the market is the best form of coordination, and that state intervention should simply correct market imperfections. ↵
- On the importation of PBF into Burundi by Dutch NGOs as early as 2002 (who even dared to propose PBF as an instrument to fight the COVID-19 pandemic, confirming the opportunistic nature of the solution) is another case often taken as example, (see Falisse, 2019) and which is very similar to the transfer processes experienced in Burkina Faso or Mali. ↵
- Note the organisation's current attempt to give even more space to the private sector in the UHC and the same selective strategy of references to support the ideas proposed, insisting, true to the NPM that "governments focus on governance of the whole health system" ((WHO, 2020b : 3). ↵
- See Dagenais' chapter ↵
- "Since poor people typically cannot buy such care for themselves, there is a straightforward case for public finance" (World Bank, 1993 : 57) ↵
- See the case of the PBF in Senegal in the chapter by Bodson and Zongo or Burkina Faso in the chapter by Beaugé et al. ↵
- See the chapter by Beaugé et al. ↵
- See the chapter by Zitti et al. ↵
- See the chapter by Bodson and Zongo ↵
- In Burundi, the PBF "allows a technocratic elite, appreciated by donors and international PBF promoters for its technical competence, to assert its place within the ministry" (Falisse, 2019 : 94) ↵
- "The radicalist/rejectionist camp, on the other hand, holds that development management is so intimately connected with neocolonialist power relations and "managerialist" control that actions taken by development managers are invariably detrimental to the interests of developing countries, and particularly of the poor residing in those countries (see Gulrajani 2010; Mowles 2010)" (Brinkerhoff & Brinkerhoff, 2013 : 377). ↵
- See Chemouni's chapter ↵
- In 2021, a journal asked me to review an article for a special issue on PBF... what a surprise to read an article written by four consultants with a total conflict of interest on the subject, without citing any scientific reference (that I knew of) demonstrating the opposite of what they dared to assert without supporting evidence. If they tried, it is because they think it is possible to publish such an article! ↵
- In the 1970s, the US was reportedly the largest donor, including $3.4 million for a rural health project in the Sine Saloum (WHO Study group, 1978). ↵
- Year of the launch in September of the Strategic Plan for the Development of Universal Health Coverage 2013-2017 and October of free health care for children under five. ↵
- https://www.banquemondiale.org/fr/news/feature/2019/10/24/doing—business—2020—sustaining—the—pace—of—reforms ↵

